Understanding blood cancer

What is blood cancer?
Blood cancer is a type of cancer that affects the production and function of blood cells. Leukaemia is a type of blood cancer. Our bodies are made up of trillions of tiny building blocks called cells. And these cells make up every part of the body, including blood. Most blood cancers begin in the bone marrow, the spongy material inside the bones and where new blood cells are produced. All blood cells begin as stem cells, which mature in the bone marrow. They then develop into the three types of blood cells: red blood cells, white blood cells, or platelets.
Blood cancer facts
- Blood cancer is the 3rd biggest cancer killer and 5th most common cancer in the UK.
- Every 16 minutes someone is diagnosed with blood cancer in the UK.
- In the UK, approximately 250,000 people are currently living with blood cancer.
How does blood cancer develop?
There are three main types of blood cancer:
Leukaemia
Lymphoma
Myeloma
Other types of blood cancer include
Myelodysplastic syndrome is a rare blood cancer type, also known as a malignant blood disorder. It occurs when the bone marrow doesn’t make enough healthy blood cells and instead makes abnormal cells that are unable to function normally.
Another rare type of blood cancer are myeloproliferative neoplasms, which start in the bone marrow. In MPN, the bone marrow makes too many of one or more types of blood cells (red blood cells, white blood cells and/or platelets).
Blood cancer symptoms
Blood cancer can affect both men and women, and symptoms can be similar for both genders. Symptoms are not always specific to a certain type of blood cancer, such as leukaemia, and can vary per individual; however, these are the most common symptoms of blood cancer to look out for:
- Fatigue
- Unexplained weight loss
- Bruising and bleeding easily
- Swollen lymph nodes
- Swollen and/or painful stomach
- Infections
- Night sweats
- Pain in bones/joints
- Shortness of breath
If you’re experiencing one or more of these symptoms, it’s very important that you see your GP and ask for a blood test. If your symptoms are a form of blood cancer, early detection can greatly improve the success rate of your treatment and recovery.
Blood cancer prognosis and treatment
Prognosis can vary depending on the type of blood cancer, the stage of diagnosis, age, how fast the cancer is progressing, fitness and overall health.
Healthcare professionals will decipher which treatments are most appropriate for the patient.
The most common forms of treatment for blood cancer include chemotherapy, radiotherapy, immunotherapy, stem cell transplant (SCT) / (bone marrow transplant) and CAR-T cell therapy. Some people diagnosed with slow-growing forms of blood cancer may not need immediate treatment, or they may never need treatment.
Blood cancer survival rate
Survival rates are dependent on the type of blood cancer and different factors, such as age, general health and the stage of diagnosis.
For leukaemia, around 55% of people live for five years or more after a leukaemia diagnosis. It’s important to remember that blood cancer survival rates are improving. Many charitable organisations, including our researchers at Leukaemia UK, are working hard in the background on research programmes to find kinder, more effective treatments for different types of blood cancer.
If you are worried or concerned about a blood cancer diagnosis, take a look at these informational resources and links to additional cancer charities which may be able to support you.
In addition, we highly recommend that you talk directly to your GP about any concerns you may have.
Learn more about blood
Blood is essential to life. Blood circulates through the body and has many different functions, including:
- transporting oxygen and nutrients to the lungs and tissues
- forming blood clots to prevent excess blood loss
- carrying cells and antibodies that fight infection
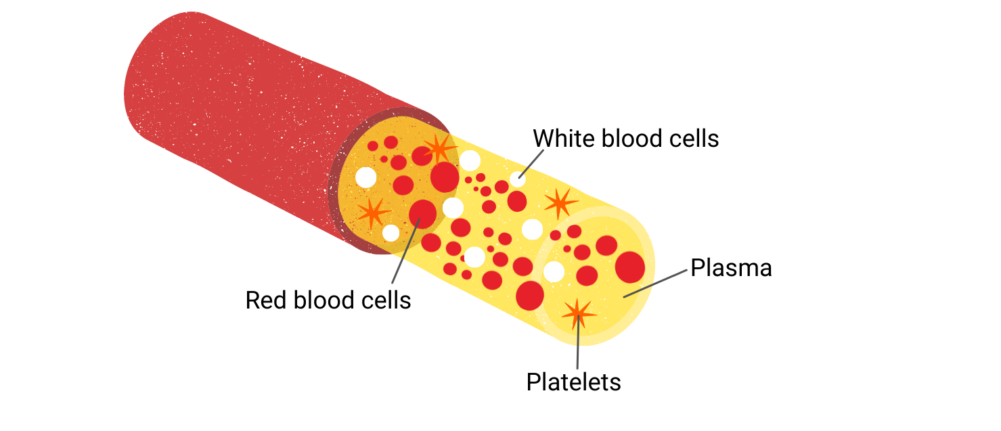
Blood consists of liquid and solid components. The liquid part, called plasma, consists of water, salts and protein. Over half of blood is plasma. The solid part of the blood contains red blood cells, white blood cells and platelets.
Blood cell production
Blood cells are being made all the time, new blood cells to replace old ones that have worn out and died off. The new blood cells are made in the bone marrow and the process starts with a stem cell – an immature cell that can develop into all types of blood cells. In a healthy person, the system of blood cell production is finely controlled in a process called haematopoiesis.
Composition of blood
Red blood cells
Red blood cells have an important function to transport oxygen to and from the lungs. The life span of a red blood cell is approx. 4 months, and they are regularly replaced. The human body produces around 2 million blood cells every second.
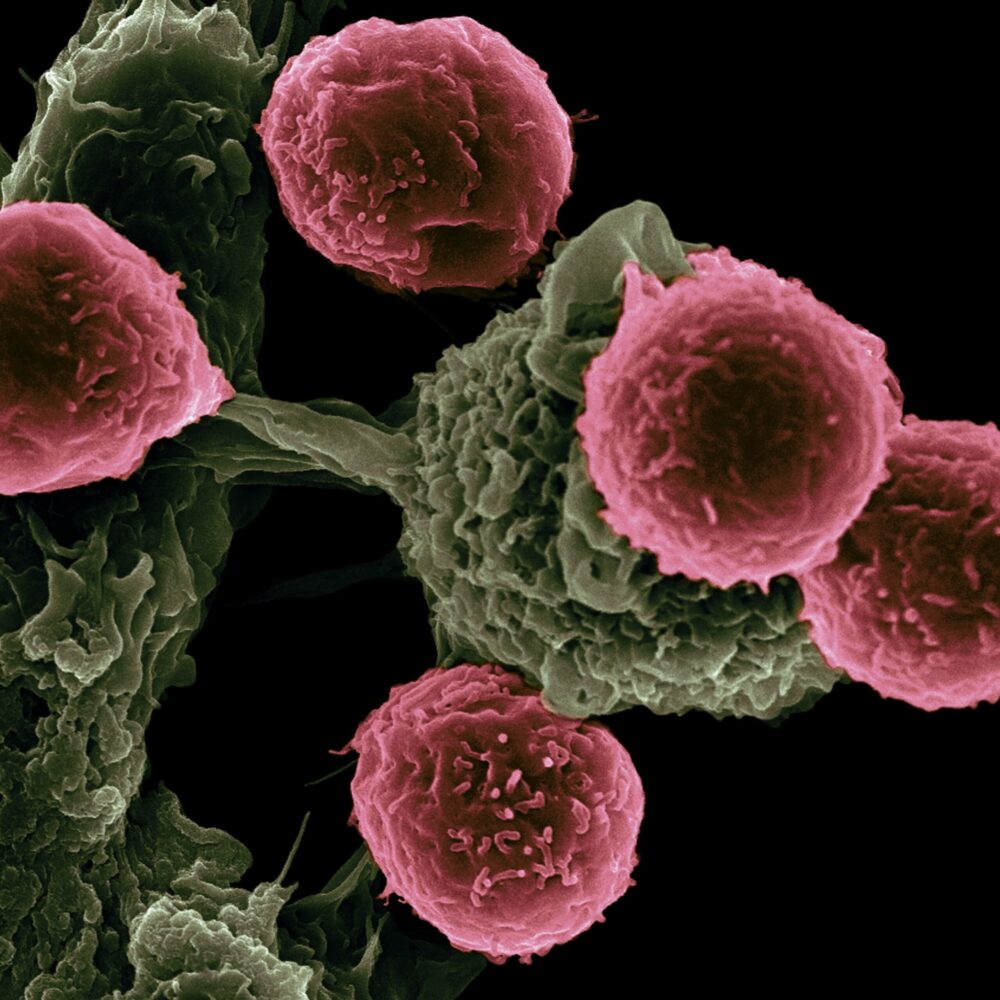
White blood cells
They flow through the bloodstream and attack foreign bodies, like viruses and bacteria. They can even leave the bloodstream to extend the fight into tissue. The number of white blood cells in a microliter of blood usually ranges from from 4,000–10,000. Higher or lower levels of white blood cells can indicate disease.
Platelets
Platelets receive that signal, travel to the area and transform into their “active” formation, growing long tentacles. They make contact with the blood vessel to form clusters and plug the wound until it heals. There are usually between 150,000 and 400,000 platelets per microliter of human blood.
Plasma
Plasma is yellowish in colour and is mostly made up of water (92%), but it also contains proteins, sugars, hormones and salts. It transports water and nutrients to the body’s tissues.
How cells are made
When the stem cell divides, it can either produce more stem cells or other immature blast cells that develop into mature blood cells over time. In this process of specialisation, immature blast cells become either lymphoid or myeloid cells.
Lymphoid cells are a type of white blood cell. They help fight infection, and they include B lymphocytes and T lymphocytes.
Myeloid cells go on to form red blood cells, platelets and other types of white blood cells such as monocytes and granulocytes.


Searching for answers – Leukaemia UK funded research
Dr Miguel Ganuza: 2020 John Goldman Fellow whose research is specifically interested in clonal haematopoesis (CH), where blood cells may accumulate with mutated DNA that are derived from one single mutated cell.
“My major aspiration is to contribute to the discovery of new treatments to prevent the development of different types of leukaemia.”
References
*Factors which may increase the likelihood of blood cancer – Source: Blood Cancer UK