
30 Sep 2016
Jimaine’s acute myeloid leukaemia story
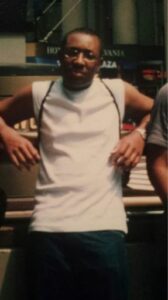
Jimaine was treated for acute myeloid leukaemia (AML) at King’s College Hospital 18 years ago. Today, Jimaine – AKA Je’Londen – is a professional musician and is set to release an album inspired by his blood cancer journey. Here, he tells his story.
How I discovered I had AML
 I was diagnosed when I was a teenager. I was going to school and getting sick every day. One week I had the flu, the next week I had tonsillitis, then I’d break out in rashes or have bumps on my skin. I never usually had issues like that.
I was diagnosed when I was a teenager. I was going to school and getting sick every day. One week I had the flu, the next week I had tonsillitis, then I’d break out in rashes or have bumps on my skin. I never usually had issues like that.
I went to my GP every week, to the point where they got annoyed with me and sent me away. They’d give me pills and say, “Go home, take some time off, you’ll be fine. You’ve just got tonsillitis.”
I asked them if I could have a blood test and they said, “It’s not necessary. You’re so young, there’s nothing wrong with you.”
One day, my neck was hugely swollen and I was told it was my glands. I thought it was glandular fever or something like that. I didn’t think about leukaemia.
I was rushed to A&E where I had a blood test, then they sent me home. The next day, somebody called me from the haematology ward and asked me to come in for a couple of days because they wanted to do more tests.
I packed my bag for a couple of days but ended up spending nine months there. That’s when they diagnosed me with acute myeloid leukaemia.
The shock of diagnosis
It started with lots of different blood tests. They told me they had to start chemotherapy right away because I had probably had leukaemia for several months without realising. They had to treat it aggressively because they said I didn’t have much time left and I would need a bone marrow transplant.
First, they checked my family members, but nobody was a match. Then they checked the bone marrow register, but there were very few black and Caribbean people on there at that time. Instead, they decided to harvest my own bone marrow cells, give me chemotherapy to knock the remaining cells down, then give the harvested cells back to me.
They started giving me chemotherapy and put me on the adult wing because they didn’t have space on the children’s ward.
I went through a very deep depression because I didn’t really understand what was going on with my life. Also, I was having all the symptoms you have when you have chemotherapy – my hair started falling out, I was getting sick, I lost a lot of weight and my skin was peeling.
It was very tough because before I was diagnosed, I was in my prime. I had just learned to drive and was planning to get a job, move out and start my life. I had a record deal and was going to the BRITs School for performing arts.
Then they told me I only had six months to live.
I was heartbroken because I was about to have this music career, and I saw people who went to the same school as me, like Jesse J and the Floetry, getting signed. I had thought that was my moment, then it was all taken away from me.
A tough treatment journey
 There wasn’t anything on the ward for people to do to entertain themselves and take their mind off the treatment. No TV, no radio, no wifi. I felt like I was in prison.
There wasn’t anything on the ward for people to do to entertain themselves and take their mind off the treatment. No TV, no radio, no wifi. I felt like I was in prison.
Your immune system is really low, so you can’t go outside. And you can’t leave the ward unless it’s for an X-ray or something, so I had to be in the room all the time. It was very, very traumatic for me.
I started to blame everybody else. I didn’t want people talking to me. I didn’t want nurses touching me. I didn’t want doctors coming in.
I struggled with the treatment cycle too, because I didn’t really understand it. They would give me a course of chemotherapy, then I’d think it was over. My white cells started coming back up, and they’d tell me I could go home, so I’d think the treatment was finished. Then they’d tell me I had to come back in three weeks to do it all over again.
The doctor who made a big difference
It was a constant cycle like that for a year and it really took a toll on me.
I was very fortunate to have Professor Mufti caring for me. He was more than just a doctor and kept me going. He and my dad became close friends too.
He would come in in his jeans with his son on a Saturday to see how I was doing. I’d never seen him in jeans before. Before he left, he would say, “Everything all right? If you have any problems come to me.” He was like an uncle who I could complain to, be angry or cry with without feeling like I was being judged.
Remission, relapse and the search for a donor
After that, I was in remission for a year and I went to college to do IT. During a monthly check-up, Professor Mufti told me I’d relapsed and had to be admitted to the ward straight away. I came for my blood test in the morning and they basically told me, “You can’t leave. You have to go upstairs.” I was literally only out of hospital for one year only.
So I was back in prison again, and this time they told me they couldn’t give me any chemotherapy because I had so much the last time. I couldn’t have radiotherapy either. I needed a transplant from an unrelated donor.
I was told by the doctors in the beginning that due to my ethnicity I had a 1, in 900,000 chance of ever finding an unrelated donor with basically more chance of me winning the lottery.
That is why I chose to come forward and give my story to the press in order to get more people out there to join. I did not want to die in vain and chose to stand for something. So we went on ITV and Choice FM, which was the “urban” radio station at the time. I did a lot of interviews with them and some newspapers. We had donor drives in America as well.
It took a real battle to find one and a lot of black and other minorities never find a match. We found a donor in America and I went through the second transplant. I was one of the blessed ones. It’s important that more people join the bone marrow register.
After that, I had to reboot my confidence because I didn’t look the same as I had before treatment. It took me a while to heal from the chemotherapy – my face had swollen up, my complexion was darker and my hair didn’t grow back the same.
Getting back to being an artist
The positive side of all this is that I became a songwriter. After my diagnosis, I had so many things to sing and talk about and people were giving me opportunities to write. Everybody kept saying, “You should go to America.” So I went, and the response was positive.
I’ve had publishing deals writing for others. Now I’m getting back to being an artist and I’m working on an EP.
It’s a nine-song EP, it’s very positive and it tells my story. It’s a mixture of Afro beats, R&B and pop music, with a little bit of reggae – the music I grew up listening to.
I want to inspire people. I want it to say, “I overcame. You can overcome too.” But that doesn’t mean you have to overcome cancer. It could be things like bullying or dealing with hateful, hating people.
It’s very inspiring and rewarding and it’s motivating me. For ages, I put it off because I thought nobody would want to see me as I was. But everyone said, “You’ve got to do it, you’ve got to do it.” And when I come to hospital for my check-ups and talk about it, people say, “Yeah, you need to share your story. What took you so long?”
We’re really grateful to Jimaine for sharing his story and wish him all the best with his new album.
Read more stories from others affected by blood cancers here
You can help Leukaemia UK continue to make a difference to those affected by blood cancers by donating here
Related posts
25 June 2019
Championing groundbreaking therapies and emotional support
We are proud to be at the forefront of funding innovative research into gene therapy treatments
6 June 2022
An open letter to people with a weakened immune system
Leukaemia UK joins the NHS and other charity leaders by signing an open letter, to encourage people with a weakened immune system to continue to book in or visit a walk-in centre for their Covid-19 vaccines.
21 June 2023
Prestigious jointly-funded fellowship could be catalyst for myeloma prevention
Dr Louise Ainley, University College London, has been awarded a Clinical Research Training Fellowship – jointly funded with the Medical Research Council. The three-year project is set to investigate which…
21 August 2023
Jelly bellies, yellow teeth and hairy ears – parents reveal the most EMBARRASSING questions their children have asked
A new survey has revealed the most embarrassing, awkward and often hilarious questions that parents or grandparents surveyed have been asked by children. The survey was undertaken by charities Leukaemia…